Case Study: Moderna
Develop: An Experimentation Mindset - Prototyping: From Exploration to Validation
Learning Objectives:
- Explain how the type of prototype changes as critical questions are answered and the prototyping process advances
In 2020, as the COVID-19 pandemic began to spread across the world, scientists at Moderna were developing a vaccine using innovative technology: messenger RNA, or mRNA. Instead of injecting a weakened or inactive virus into the body, the mRNA vaccine acts as information: It instructs muscle cells to produce harmless proteins that will trigger an immune response.
The COVID-19 pandemic disrupted life across the globe, and Moderna’s innovative vaccine was urgently needed by billions of people. But Moderna was a small development company, so the unprecedented desirability of its innovation was also an unprecedented logistical problem—not only high impact, but incredibly high difficulty.
For a company like Moderna, what do you think would be the biggest challenge surrounding such a large global vaccination effort?
- Distribution
- Manufacturing
- Research
- Sales
Distribution and the other factors would all be challenging, but the following video transcript will discuss manufacturing.
As Moderna CEO Stéphane Bancel explains in the following video transcript, the need to boost manufacturing to produce a billion vaccine doses was an unprecedented challenge, especially for a development company.
STÉPHANE BANCEL: My name is Stéphane Bancel. I’m the CEO of Moderna.
The piece that was an extraordinary challenge for us was manufacturing, and the reason is the following: we were not a commercial company. When the virus hit, I was first made aware of that virus at Christmas 2019. In 2019, we had made less than 100,000 vials for the entire company across all the products we had—less than 100,000 vials. We were a development company.
I came back from the World Economic Forum in Davos the week of January 20th, 2020, convinced 100% that this was going to be a pandemic like the 1918 flu. I walked into the office upon my return from Davos, with a little swing by Washington. Because of that conviction, I went to see Dr. Fauci, the FDA, and other US agencies to say, “Guys, it’s going to be a pandemic. We need to hurry up.”
I came back to Boston and went into the office of Juan, who was leading manufacturing. I told him to sit down because I said, “You need to sit down; you’re going to have a mini heart attack.” Then I said, “How do we do a billion doses in arms in 2021?”
He looked at me and said, “You’re asking me how we do 10,000 times more product in 12 months’ time from now?”
“Correct. You are correct,” I replied.
He said, “How do you think people will react if you go to a car manufacturer or Apple and you tell their teams, ‘We have to make 10,000 times more product next year?’”
I said, “I think they’ll think I’m crazy.”
He said, “Yes, I think you’re crazy.”
I responded, “OK, now that we are done with that, I need you to tell me: what do you need to make it happen? We’ll find the resources, but I believe a vaccine will work because of all the work we have done before in nine other vaccines in the clinic. And we’re going to need a billion doses next year to help as many people as we can on the planet.”
Before we explore how Moderna solved this problem, let’s examine the background: How did Moderna empower its scientists and researchers to prototype a vaccine so quickly?
When the pandemic struck in early 2020, Moderna had already been working for years on mRNA technology. This technology was considered a risky venture in the healthcare industry because many scientists were unconvinced it could work.
In the following video transcript, Stéphane Bancel explains the appeal of the innovation concept.
STÉPHANE BANCEL: The reason I got excited about the potential of the impact that mRNA could have is that if you think about the central dogma of biology, think about DNA as the hard drive of life. It stores all the instructions for all proteins in your body.
But the way your cells make protein—like your pancreas making insulin, for example—is by copying the instruction just for insulin from your hard drive (the DNA) into a molecule called messenger RNA (mRNA), which everybody knows by now. That molecule is then translated into a protein—in this case, insulin—which your body needs to be healthy.
So, the concept was: could you make a synthetic messenger RNA in a factory that you could design with the instructions for a protein you wanted, whether for a therapeutic purpose or, in the case of a vaccine, a preventive effect? Then you would inject that into a human body.
This concept opens incredible possibilities—hundreds or thousands of drug candidates, helping people across any therapeutic area imaginable. It’s a very impactful way to help people, and that was the first attraction.
The second attraction was the fact that mRNA, if you think about it, is an information molecule. The mRNA we inject into people is never a drug. It carries instructions, information for your cells to make their own drug using the same machinery they use all the time just to stay alive.
We knew that if it worked once, it would work for many of our applications. That was very powerful in terms of the probability of success for a drug. As we know, most drugs based on traditional pharmaceutical technology fail in clinical trials.
The other piece, which I think is vastly underappreciated by people—even in our field—is that the raw materials we use for this data exist in nature. We do not make them up.
When you think about toxicity, which has been the biggest issue in the industry for 150 years, if you can make a safe mRNA molecule work once, it’s going to work again because the building blocks of mRNA are the same.
So far, Stéphane Bancel has explained two aspects of the concept’s desirability: the numerous possible therapeutic applications of mRNA, and its lack of toxicity. Soon, he will explain additional desirability factors.
But first, let’s explore some critical assumptions to be tested around feasibility and viability:
- Feasibility
- Will the body reliably respond to the synthetic mRNA’s instructions?
- Can Moderna attract the talent to produce successful mRNA treatments?
- Viability
- Can synthetic mRNA be produced quickly and at a low cost?
Whether the mRNA will work in the body, and whether Moderna will be able to function by attracting the right talent, are feasibility questions. Producing mRNA at the right cost is a long-term viability question.
STÉPHANE BANCEL: The fourth piece that was really exciting to me is speed.
During my training at Lilly and watching the pharmaceutical industry over the last 25 years of my career, I’ve been very frustrated—like many of my colleagues—about the pace at which things move. From an idea to a drug in the lab, to a drug in the clinic, to a drug being approved, the process takes a painfully long time. As we all know, it can sometimes take 5, 10, 15, or even 20 years to go from an idea to approval. That is awfully long, with many people suffering meanwhile.
But think about mRNA. If mRNA is an information molecule, and it’s just about the order of our four letters on the message, it’s always the same way to make it. We don’t have to invent for every product—like in the case of pharmaceuticals—how to make it safely at a big commercial scale. It’s always the same process.
And then the icing on the cake is manufacturing cost. We believe manufacturing costs should be low because we do not use cells to make our synthetic mRNA. It is a liquid-phase process—i.e., in water—using enzymes. This process is highly scalable and much cheaper because you can concentrate the reaction and end up with very small reactors.
So, if you look at all those attributes:
• A new technology that could make hundreds or thousands of drugs that cannot be made with other technologies
• A higher chance of approval
• Faster and cheaper development
Initially, this looked too good to be true. But the more time I spent with Nobel Prize winners and scientists examining this opportunity, the more convinced I became.
Eventually, I told myself—and my wife—that I needed to take a chance and try to build this company. Because if we could find a way to make this work safely, it would impact millions of people.
Moderna took a risk and recruited the talent to explore synthetic mRNA as an innovation. However, the innovation concept involved more than just the mRNA itself. Moderna would also develop software to help scientists request the mRNA sequences in multiple ways at once.
Review the following diagram of Moderna’s research engine.
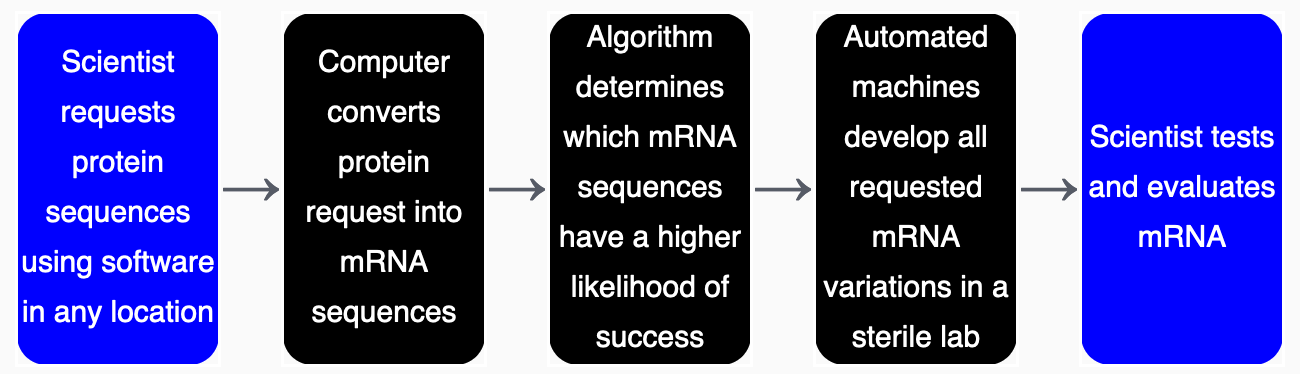
You could say that the research engine demonstrates multiplication because the data is processed twice: The first process converts the protein sequence to an mRNA sequence, and the second process applies a machine-learning algorithm to sort by likelihood of success. The qualitative change is that the second step is analytical.
This is a complex example, and Stéphane Bancel explains more in the following video transcript. While Moderna did not apply multiplication to develop the research engine, this is an example of how there are recurring patterns (task unification, multiplication, etc.) in most innovative offerings.
STÉPHANE BANCEL: So we built this super cool software tool that is available on our website as a short three or four-minute video that you can check out.
With this tool, scientists—whether they’re on an iPad, a laptop, or sitting on a sofa—can literally design any drug they can think of. They can create variants of that drug by trying different mutations of amino acids, lipids, mRNA chemistries, or manufacturing processes to test various scientific hypotheses.
For example, if a scientist wants to work on an HIV vaccine and has 20 different ideas for potential vaccines but doesn’t know which one is best, they can design all 20 variants on their computer at the same time. This process can take as little as 10 minutes or several weeks—depending on how much thought they put into it—and they can save their progress to revisit later.
Once they’re ready, they click “order,” much like adding items to an Amazon cart. From there, the process is entirely digital—zero human intervention. The order is sent directly to a set of robots at our Norwood, Massachusetts facility.
We’ve built an army of robots that automate everything, including robots that move plates between other robots. This allows us to industrialize the process, eliminate human errors, and scale efficiently. All quality control is also fully automated.
At the end of the process, the scientists receive their vials in a couple of weeks, ready to test their ideas in the real world.
This research engine represents the muscle and processes within our company, enabling us to go from an idea in someone’s brain to a drug in a vial—as many as needed—in just a matter of weeks. In the world of pharmaceuticals, this is total science fiction.
When mRNA vaccines proved successful, Moderna had a major innovation opportunity in the healthcare space. Then the COVID-19 pandemic occurred, bringing its numerous logistical challenges.
Moderna solved these challenges by adopting the same experimentation mindset that we have explored, asking the following: What is the quickest path to the experience?
To increase the scale of vaccine production so quickly, Moderna needed to hire thousands of people. Training itself is often a form of prototyping for certain kinds of workers.
STÉPHANE BANCEL: So I’m sure you’re wondering, how did we manage to produce 10,000 times more product from a manufacturing standpoint?
In our industry, there are four big things you need to solve for:
1. Clean space (clean rooms): You need controlled environments where production can take place safely.
2. Equipment: You need the machinery to drop into those clean rooms.
3. People: You need a trained workforce to operate that equipment.
4. Raw materials: You need a consistent supply chain for the materials used in production.
What we did was immediately reach out to our suppliers and tell them what we needed. Unsurprisingly, most of them were initially shocked. Many said they could try to meet the challenge, but they required payment upfront because scaling their capacity to this extent meant buying new machines and hiring additional staff.
For smaller suppliers, there was a real risk of bankruptcy if our vaccine failed in clinical trials. But we worked closely with them to ensure they were willing to take on the challenge.
Building new plants or clean rooms was out of the question—we simply didn’t have the time. Instead, we identified the top five contract manufacturing companies in the world that already had the space we needed. Ultimately, we partnered with Lonza because many other companies couldn’t meet our timeline. If someone told us they would have space available in two years, we politely thanked them and hung up the phone. In a pandemic, that wasn’t an option.
Next, we tackled recruitment and training. Thousands of people had to be hired simultaneously and trained quickly. To do this, we created a mock factory in a separate building, complete with duplicate machines. This setup allowed us to train new recruits without interfering with the production happening in the actual GMP (Good Manufacturing Practice) suites.
This approach ensured that when new workers stepped into the clean rooms, they were already well-prepared to operate the equipment effectively.
As Stéphane Bancel explained, Moderna built a replica of their factory, with mock equipment, specifically for training purposes—this allowed them to not only proceed with speed, but also assess the training in a single facility and adapt it as necessary.
This is also an example of multiplication because one factory is a copy of the other, but with a qualitative change: one has real equipment, while the other has mock equipment only for training.
From development, to contracting with suppliers, to manufacturing, Moderna faced a number of challenges in suddenly and unexpectedly ramping up production of its vaccine. However, these challenges were overcome in part because of innovative problem-solving related to clarifying, ideating, and prototyping solutions.